Researchers from Harvard and MIT are Working Together to Develop a Face Mask that can Light up When it Detect Coronavirus
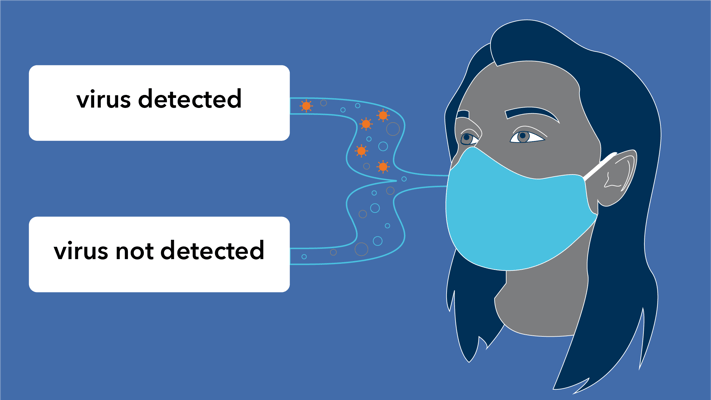
Image credit: ALLEN INSTITUTE
Globally, COVID-19 is rapidly spreading and trials are on their way to develop a potential antidote/vaccine of COVID-19. It is expected that for an antiviral drug/vaccine to pass all the trials and to become available in a useable form, it will take 12 to 18 months. Until then tracing, tracking, and isolating the affected persons is the best way to curb the spread of coronavirus. There exist many ways by which we can test coronavirus. Among all, a prominent and most-performed technique is polymerase chain reaction (PCR). It uses the swabs taken from individuals’ noses and throats and detect the viral RNA.
But the PCR method also have its own limitations like test kits are only available for a fraction of people that need to be tested, requirement of trained and skilled manpower to perform the tests, the requirement of specialized laboratory equipment, and significant time to be performed.
For the fast, easier and safe detection of coronavirus, researchers James Collins, Peter Nguyen, and Nina Donghia, and Luis Soenksen at the Wyss Institute are developing a rapid self-activating COVID-19 diagnostic face mask which can detect coronavirus when an affected person wears it.
Back in 2016, The team lead by James Collins has already developed a low-cost sensor tool that can detect Ebola and Zika.
In the case of COVID-19, they are adjusting the existing tool to detect the coronavirus. The team is designing a face mask that can light up when it detects coronavirus by using fluorescent signals. The team is designing a face mask such that it can produce a fluorescent signal when a person affected with coronavirus breathes, coughs, or sneezes.
Collin's lab highlighted that though the project is in an initial phase, the preliminary results are promising. The team has been working on the sensors' ability to detect the novel coronavirus so they can increase its sensitivity and detect coronavirus in a small saliva sample.
The technology used by Collin's lab is already a proven right technology. Earlier in 2018, they demonstrated that the lab’s sensor could detect viruses that cause SARS, measles, influenza, hepatitis C, West Nile, and other diseases.
This new face mask sensors consist of genetic material - DNA and RNA - that binds to a virus. The genetic material is freeze-dried onto fabric using a machine called a lyophilizer. This process will suck all the moisture out of the genetic material without killing or hampering it. Such a design can remain stable at room temperature for several months, giving the masks a relatively long shelf life.
The newly designed sensor needs to detect only two things. One is the sample from the person like saliva or mucus and the other is virus genetic sequence.
Now when they detect the coronavirus in the sample, they are expected to give off a fluorescent signal within one to three hours.
Also, previously Collin’s team developed a sensor that can change from yellow to purple when a virus is present. So the researchers of the team are also discussing to apply the same sensor technology in the case of coronavirus.
To quantify the presence of fluorescent light, they used a device called a fluorimeter.
This face mask can be worn by patients or individuals at home. If the person is affected by coronavirus then the face mask will light up. This light-emitting face mask could rapidly signal out the presence of the virus even without any need of hands-on manipulation, or external chemical reaction. The face mask will show up the signal as soon as it detects the coronavirus from the infected person so the patients can be quickly triaged for proper medical care and healthcare workers, other persons nearby will be protected from coronavirus.
A similar type of sensor that the lab designed, in 2016, in the case of Zika was estimated the cost of about $20 each and they can give results within two to three hours. So, we can expect, the newly designed sensors in the case of coronavirus might offer a cheaper, quicker, and more sensitive form of detection than traditional diagnostic tests.
The sensors might offer a cheaper, quicker, and more sensitive form of detection than traditional diagnostic tests. The lab's sensors for Zika, for example, can diagnose patients within two to three hours and the estimated sensor cost was about $20 each, while the test itself was $1 or less to manufacture.
